Health care providers of East Carolina University’s Healthier Lives initiative in the Brody School of Medicine continue to use the program to address health care needs for children in rural eastern North Carolina counties and are finding pathways to expand access to care at schools in Duplin County and beyond.
The Healthier Lives at School & Beyond Telemedicine Program originally launched in 2018 to deliver interdisciplinary services virtually to rural school children, staff and faculty during the school day. In response to COVID-19, the program continued to address health care needs for children and expanded access while students were learning remotely.
Since the fall of 2020, the program has used an ECU Transit bus to visit schools in Duplin, Jones and Sampson (Clinton City Schools) counties to provide high-quality health appointments. The retrofitted motorcoach has been used to provide screenings for 303 students, with additional visits planned for existing program partnerships and newly established ones.
The initiative was recognized recently by the Mid-Atlantic Telehealth Resource Center with the Breaking Barriers Through Telehealth Award in the category for small, rural and safety net organizations. During the 2024 Rural Health Symposium, a presentation on Healthier Lives – On the Road Again: Rolling to Reduce School Suspension – was awarded first place in innovations panel.
Experiential learning
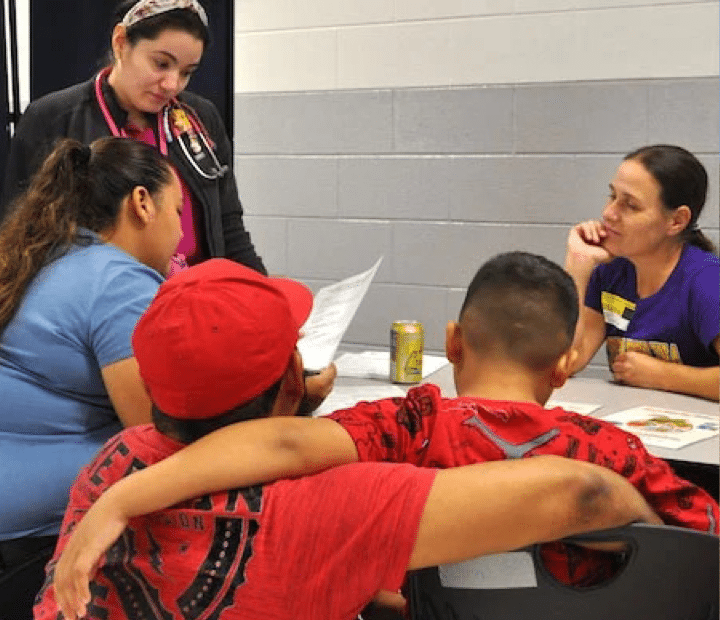
Delivering care in the community is also delivering learning opportunities for ECU students. Third- and fourth-year medical students and medical residents participate in clinic days, gaining hands-on experience providing health care to rural populations.
Recent Brody graduate Dr. Melenis Lopez said the Healthier Lives clinics demonstrate that service is truly ECU’s mission. During a school clinic in the fall, Lopez applied pediatric learning experience as a care provider. She collected patient history and assisted in making plans for children that could be passed on to the school.
“Providing care in a place that is convenient to the community can be lifesaving,” Lopez said. “Offering physicals can uncover developmental delays and health problems. Children can’t stay in school without these physicals and proof of vaccinations, so I’m happy we were able to be there for the kids.”
Lopez and her ECU cohort guided elementary students and their families through clinic stations to take vitals, check vision and hearing, and perform physical exams. Students could meet with mental health and nutritional professionals for additional screening when needed.
Lopez used her ability to speak Spanish to help the children feel comfortable and ease the burden on families who may not understand the forms or instructions from the care provider.
Rural health care
Dr. Krissy Simeonsson, associate professor for pediatrics and public health and the medical director for the program, is proud that Healthier Lives is giving ECU students the opportunity to experience health care in a rural setting.
“Students can see that they can help,” Simeonsson said. “Most students and residents we’ve had have that ‘aha’ moment and can see themselves in primary care. They realize they can succeed out here.”
Jill Jennings, ECU’s Healthier Lives program manager, said the hybrid approach of on-site clinics and telehealth makes it easier for the medical providers to communicate with parents in person and more readily make referrals for any nutrition or behavioral health follow-up virtual care.
A $1.2 million grant from the Health Resources and Services Administration funded the first four years of the program. Funding now comes primarily from Anonymous Trust, a private North Carolina foundation, and has been provided by the Harold H. Bate Foundation, the ECU Health Foundation, and the North Carolina Department of Health and Human Services Office of Rural Health.
“There are many opportunities for institutions such as ECU to leverage their resources to address community needs,” said Debbie Aiken, executive director of Anonymous Trust. “This initiative is a wonderful example of ECU recognizing health care disparities, and in partnership with a local school district, serving children who might otherwise not receive the care that they deserve.”
Aiken witnessed a program clinic in action at Rose Hill-Magnolia Elementary School in Duplin County. ECU medical students and residents, health sciences undergraduate and graduate students, Healthier Lives team members and partners from the school system and Duplin Health Department screened 47 students who otherwise would have been suspended for not having a health assessment completed by a medical provider.
“These partnerships should be happening across the state,” Aiken said. “Seeing it helps you truly understand the disparities in our rural communities. If more school systems understood that this is available, they would want to participate.”
Community engagement
Dr. Jenelle Brison ’24 said Healthier Lives provided an opportunity for community engagement for medical students. Brison encouraged fellow Brody students to participate.
“It’s so nice to interact with the little kids,” Brison said. “Events like this help break down barriers and offer unique training for students.”
While Brison ultimately hopes to focus on obstetrics and women’s health, she was at ease helping children with vision screenings and demonstrating a blood pressure cuff before taking vitals.
Dr. Bolu Aluko ’24, a Tiana Nicole Williams Scholar at Brody, was drawn to the opportunity for community engagement provided by Healthier Lives.
“Coming into the community is incredibly enriching,” Bolu said. “Every med student should do this. It’s a fantastic way to serve and practice our clinical training.”
Through an interpreter, the family of one student said they had received a call from the school that their son would not be able to return to class because he had not had a physical or proof of vaccinations. They had just moved from Mexico to Warsaw, North Carolina. Without the availability of a Healthier Lives clinic at the school, they would not have had access to a health screening for their son in time to meet the state-mandated deadline.
The family sat with an interpreter and was provided a nutritional referral and a connection to a primary care clinic in Warsaw to establish a medical home. “We’re grateful to know he’s healthy,” his mother said through the interpreter.
“You have to meet people where they are,” Simeonsson said. “A lot of families trust the school. When you see the families getting help for their children, you know the program is living up to expectations.”
Layah Collins is like any other kindergartner, bubbly and full of life. But in 2019 and over the next five years, she would endure unimaginable pain and suffering from Neuroblastoma. But her mother says with help of the doctors and nurses at the Maynard Children’s Hospital, it’s a battle Layah would fight and win.
“Girl on fire.” 6-year-old Layah Collins says that’s her favorite song. Ironically, it also describes her incredible journey in her fight against cancer.
In 2019, 1-year-old Layah was diagnosed with stage four Neuroblastoma. Her mother, Alysha Collins, says she found out after a scan at the Maynard Children’s Hospital revealed a bump on her head was actually a tumor.
To donate to the Children’s Miracle Network in Greenville — Click Here!
“I was shocked not what I was expecting. It’s one of those you see the commercials on TV but you never think it’s going to be your child,” says Collins.
Enter Dr. Cathleen Cook, a woman who Alysha says not only became their physician, but an honorary member of the family and would stand by her and Layah’s side from that moment on.
“On my fridge, on the top part, I have when she was diagnosed and all the pictures that she has shared and given to me. So, my son even knows who Layah is, so we do get very close to our patients,” says Cook.
By 2020, 2-year-old Layah had seven surgeries, five bone marrow biopsies, one specialized radiation session, one stem cell infusion and thirteen cycles of Chemotherapy. It was then that Alysha says it became apparent the disease was winning and she was forced to make the hardest decision she’s ever had to make and stop treatment.
“Nothing was working and the treatments made her sick, she was nauseous, she threw up, she had lost all of her hair, her beautiful curls had all fallen out and I just wanted her home because if it wasn’t working I didn’t want to keep putting her through that. She was only 2 and her little body had already been through so much,” says Collins.
Alysha says, however – her daughter did live and thrive – and over the next three years frequent scans showed the cancer was not growing or spreading.
The relief was short-lived — in 2023, tests showed new sites of the disease not previously seen. That’s when 5-year-old Layah would undergo yet another brain surgery and be given a different Chemotherapy agent, referred to as compassionate use medication.
The new treatment worked — and in January 2024 6-year-old Layah’s scan was negative. Alysha says it is nothing short of a miracle for her daughter to be in remission for the first time in five years.
“I was like what does this mean and she said that she would be considered in remission, and I just cried, because those were words that I never thought I was going to hear,” says Collins.
Alysha says although it’s been a rough road, she’s grateful for the support from all the doctors and nurses at the Maynard Children’s Hospital.
“The care here was amazing, everybody made us feel like family, still when she walks through the front door everybody knows who Layah is, everybody knows,” says Collins.
She says Layah is stronger than ever and living the life that she deserves.
“This girl is on fire. She’s walking on fire. This girl is on fire,” says Collins.
Dr. Cook says Layah is in remission and there are no new signs of the disease. She says Layah will receive scans every three months for the next couple of years and continue to be monitored through age 25.
You can continue to make miracles like Layah’s happen when you tune in and make a pledge this weekend during the Children’s Miracle Network Telethon.
The neonatal intensive care unit at Maynard Children’s Hospital, also known as the NICU, is where the most delicate babies who need the highest level of care and attention come.
Most of them are premature babies who are born locally in Greenville or from 28 other counties in the east.
Premature babies born under 30 weeks or that weigh less than 1,500 grams come into this world with many risks, including retinopathy of prematurity.
“Where the blood vessels of the retina do not form normally,” Dr. Ostrovsky, the Chief of Ophthalmology Services at ECU Health System explained.
To donate to the Children’s Miracle Network in Greenville — Click Here!
The retina contains the photoreceptors in the eye, making it crucial to see normally.
So, every day and every hour matters to babies born with this condition.
“Sometimes untreated, it can cause retinal detachment and blindness,” Dr. Ostrovsky said.
Now, imagine if doctors can detect conditions like this beforehand and ensure a life of healthy vision that is made possible with the retina cam.
Once the doctor instills numbing drops, dilating drops, and stabilizes the baby’s eyelid with a metal speculum, the retina cam can take high-resolution, 130-degree pictures in a matter of seconds.
“Create better images of the baby’s retina, allow us to follow the more reliably, also to create a more reliable follow-up for the babies as they continue their treatment,” Dr. Ostrovsky shared.
Those images then allow doctors to monitor and evaluate a baby’s eye health.
The retina cam can also be used on normal, full-term babies, who have gone through non-accidental trauma, or abuse.
“These images are not only important clinically, again, for monitoring the progression of how these kids feel after the trauma they sustained, but also medical-legally when these images are shown in front of a judge and jury,” Dr. Ostrovsky said.
As a pioneer in this revolutionary technology, the Maynard Children Hospital’s retina cam will not only change many life trajectories but also serve as a role model for many doctors and hospitals across the country.
You can ensure equipment like that is available for kids in the east when you make a donation to the Children’s Miracle Telethon this weekend on WITN.
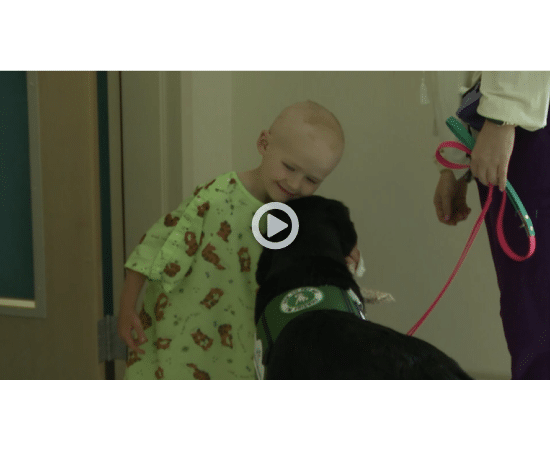
All week long on WITN, we’ll continue to share the inspiring stories of many resilient children in the east but as the 39th annual Children’s Miracle Network Telethon approaches, we wanted to show you how the recent addition of man’s best friend at the James and Connie Maynard Children’s Hospital has lifted the spirits of patients.
When you visit the Jamie and Connie Maynard Children’s Hospital, you probably expect to see patients roaming the halls but not a furry four-legged friend.
“We have patients tell us all the time, she’s the best investment this hospital’s ever made,” said ECU Health Child Life Specialist and Dog Handler, Ashton Ayers.
Meet Sam, a golden retriever, labrador, and doodle mix who’s known around the hospital for brightening children’s day.
To donate to the Children’s Miracle Network in Greenville — Click Here!
“She was going to be the best part of my day today no matter what happened,” said Maynard Children’s Hospital patient, Winter Burke.
2-year-old Sam joined the Maynard Canine Crew back in November 2023, but she’s quickly stolen the hearts of many patients.
Ayers says the love and comfort Sam provides is truly special for the children.
“As child life we’re the fun guys typically so they know us but after they’ve had 40 people in the room all day, seeing Sam is an instant smile and change in their attitude,” Ayers said.
Like many of us humans, Sam works Monday-Friday clocking 40 hours a week but for Sam putting smiles on the faces of kids like Burke makes it all worth it.
Burke says she’d been spending most her time at the hospital in bed, but seeing Sam changed that.
“I was very happy,” Burke said. “I wanted to cry because I felt like since I couldn’t see my own dog, she was like my own dog for day.”
Being in the hospital for long periods of time can be hard for any child, but with Sam there are no bad days even for Ayers.
“I say all the time since I’ve had Sam, I haven’t had a bad day at work,” Ayers said. “There’s been hard things we’ve had to deal with together, but just seeing her impact is truly amazing to see. She’s just such a cool co-worker, no one else gets to work with a dog everyday.”
Sam is so much more than just an ordinary four-legged friend to the patients at Maynard Children’s Hospital.
Some say they’re glad to have her as a safe haven because they don’t know if they’d be able to get through their individual health battles without her.
“I think it means a lot that they can make us happy,” Burke said.
Ayers says they’re now on the waiting list for another dog to add their team alongside Sam and hope your donations during this weekend’s Children’s Miracle Network telethon will help the Maynard Canine Crew continue to grow.
The Children’s Miracle Network (CMN) Celebration Broadcast honors past telethon traditions by celebrating selected miracle stories of children who represent the thousands of children in eastern North Carolina who have received treatment at James and Connie Maynard Children’s Hospital at ECU Health Medical Center this past year. This year, the CMN Celebration Broadcast will be held on Saturday, June 1, from 7-8 p.m. and Sunday, June 2, from 6-9 a.m. and 7-11 p.m. airing on longtime partner, WITN. Examples of how CMN donations are used will be featured throughout the event as well to show the impact philanthropic gifts truly make.
“We are so grateful to all those who support our Children’s Miracle Network Hospitals program all throughout the year,” said Elise Ironmonger, director of programs, ECU Health Foundation. “The generosity of our donors enables Maynard Children’s Hospital, located in Greenville and serving 29 counties, to provide life-saving care to the thousands of children who are treated each year. We look forward to being able to showcase the amazing care provided every day at Maynard Children’s Hospital during this weekend’s telethon and to have an opportunity to thank our amazing donors.”
This year’s Miracle Children and Teen include:
- Jadon Green, 1 year old, Greene County
- Leonardo Velasquez-Bartolon, 2 years old, Wayne County
- Layah Collins, 6 years old, Jones County
- Wiley Sloan, 14 years old, Wake County
The 2024 broadcast will highlight examples of the amazing care offered every day at Maynard Children’s Hospital while celebrating the miracles made possible by the life-saving care generous donations help provide. Thanks to the generosity of eastern North Carolina, thousands of children receive the specialized medical care they need, bringing them and their families the gift of hope and healing. Because of this support, the team at Maynard Children’s Hospital can ensure patients receive the best care possible.
The local Children’s Miracle Network Hospitals fundraising program is staffed and supported by the ECU Health Foundation, the non-profit charitable corporation that serves as the custodian for all financial gifts and bequests to ECU Health. The ECU Health Foundation oversees allocation of all donated funds. To donate, please call 1-800-673-5437 or visit givetocmn.com.
On the days leading up to our Children’s Miracle Network Telethon, we are introducing you to patients who have been treated at the James and Connie Maynard Children’s Hospital in Greenville. It’s because of their thoughtful care and attention that these children are so successful.
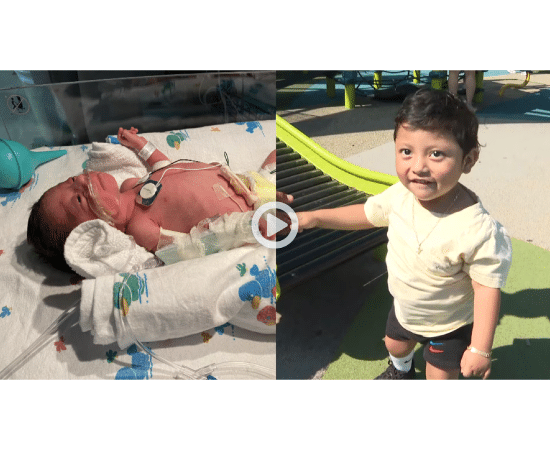
Tonight, we’re meeting Leonardo Velasquez-Bartolon – or Leo – whose struggle with a rare kidney condition left his parents thinking he might not be able to walk.
“The word that would best describe him is brave,” said Leo’s mother Vilmy Velasquez-Bartolon.
To donate to the Children’s Miracle Network in Greenville — Click Here!
Though bravery isn’t something a child should have to show, 3-year-old Leonardo Velasquez-Bartolon has harnessed it to overcome unimaginable health challenges.
“He was born prematurely in Goldsboro,” Vilmy said. “But that same day he had to be transferred over to Greenville. He was in the NICU for 20 days,”
At that point, Vilmy says they were able to take Leo home. But two months later–“I noticed that he wasn’t like a normal kid,” Vilmy explained.
They took him to a pediatrician who told them to bring Leo to the emergency department at ECU Health. He was later transferred to James and Connie Maynard Children’s Hospital in Greenville.
Leo was diagnosed with congenital nephrotic syndrome, a rare condition that can lead to kidney failure.
Shortly after Leo turned one, he had a stroke on the right side of his brain that affected the left side of his body.
“He couldn’t move his leg, his arm, and we thought that that would be very complicated, maybe he wouldn’t be able to walk,” Vilmy said. “But Leonardo is his miracle because he’s walking and he’s receiving some therapy because he’s lifting his arm more.”
Through his health challenges, Vilmy says the hospital staff always made them feel welcome and cared for.
“Everything that Leonardo has needed, the nurses have always been very, very attentive and very caring,” Vilmy said. “Every time Leo wanted toys, they would take him some toys. When he wanted cards they would take him some cards.”
Though Vilmy and her husband Pablo Morales mainly speak Spanish, Vilmy says they always felt comfortable.
“To the interpreters at the hospital, because it’s been difficult for us at the hospital because we don’t speak English,” Vilmy said. “But we’ve always had their assistance, from the interpreters.”
Leo reached a major milestone last April, he received a kidney transplant.
“It’s gone very well,” Vilmy said. “He’s been responding very well.”
At a young age, he’s survived a lot, but thanks to the care he received at the Maynard Children’s Hospital – and his own strength – he made it through.
“Right now, more than anything, I just feel proud,” said Leo’s father Pablo Morales. “I see him running, we see him smiling and laughing.”
“We doubted that he’d be able to run and do the things that he’s doing now,” Vilmy said. “But miracles can happen, and we have him.”
Pablo, Leo’s father, says Leo is mainly working on mobility on his left foot and his left arm. He is going through physical therapy to help with that process.
You can help continue to make miracles like Leo’s possible when you watch and call in a pledge during the CMN telethon this weekend on WITN.
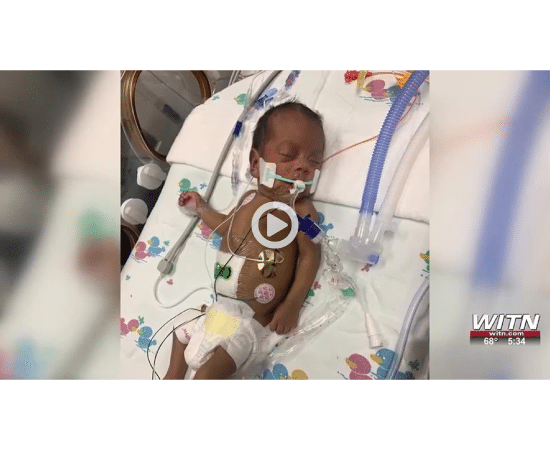
Jadon is the newest addition to the Green family. His parents feared the worst at his birth after losing two children to premature birth complications. Jadon was born in December 2022 at Maynards Children’s Hospital more than two months early. He spent over four months there with his brother, mother, and father supporting his challenging first weeks of life.
Calm, Cool, and collected is how 1 1/2 Jadon sits in the living room watching his older brother Jacob playing with toys, but that’s not how he came into the world. Weighing just two pounds, Jadon arrived around 13 weeks early. His parents Richard and Crystal Green were flooded with confusion and fear.
“We thought we had all the things in place to prevent it from happening and it was a feeling of not again,” says Crystal.
Nine months earlier, they welcomed happy and healthy Jacob to the world. His welcome arrival came after the devastating loss of a son and daughter to premature birth complications. They worried that Jadon’s premature arrival could end in tragedy yet again. It did not, as they turned to the battle in front of them.
“I’ve got a son. He’s here. He’s in NICU…. Fight… Prayer… Family… Friends,” says Richard Green.
His birth wasn’t without challenges. Jadon was jaundiced, he needed a ventilator to breathe, he was experiencing liver issues, required taking specialized formula, and needed to drink donor breast milk because of his early arrival.
On Christmas Eve, Richard and Crystal were told Jadon reacted to the donor breast milk which made him sick. Then in mid-January 2023, doctors performed exploratory surgery and diagnosed Jadon with necrotizing enterocolitis – a disease that can inflame, kill, and infect the intestinal lining.
“The way god designs the body is crazy because his body literally walled up the perforation area so that he couldn’t get sepsis and die. It stopped it, walled it up,” says Crystal Green.
Jadon’s fight to live marched on, but so did the obstacles. Jadon had a colostomy bag and central line port that became infected from the surgery, a breaking point for his mother.
“When I came back, not even 12 hours later, he looked like the Michelin Man, a totally different child,” says Crystal Green. “And I was like, why did I do this to my baby?”
But the storm clouds that had been part of Jadon’s first several months of life would finally part thanks to the steadfast care of his doctors and nurses, and the beads around mom’s neck document just how far they’d traveled on this journey.
“We actually have one of the first complete sets,” says Crystal.
The Maynards Children’s Hospital Hand to Hold Milestone Bead Program, specifically for parents in the NICU, documents every week, step forward, and landmark moment of their baby’s journey in the hospital.
And a hand Jadon had to hold himself. His older brother, Jacob, was there every step of the way, too.
“Jacob was there and the isolette was open,” says Jadon’s Father Richard Green. “It was the first time Jacob was able to interact with him, and the first thing he did was grab his hand”
The nurses and doctors at Maynards Children’s Hospital were all there with them until the final moment of their 119th day.
“They surprised us,” says Richard. “When we went in, they made stay in there and when we come out… every nurse and doctor were holding banners and saying graduation home. Not just for Jadon, but Jacob as well. When we walk all the way out… when we finally walked outside and watched him take his first breath of air outside… there was no better feeling in the world.”
Now he watches and learns from his older brother, catching up to him one step at a time. The next step for Jadon is learning how to walk. He’s starting physical therapy soon and attending Mayndards Children’s Hospital for regular check-ups.
ECU Health is working to make sure all of Eastern North Carolina is healthy in not only body but also mind.
It hosted its 12th annual Mental Health Expo on Tuesday. Hundreds of people stopped by to get resources and learn from health professionals. There were 50 local organizations to show the importance of mental health.
“Mental health is health, right? And mental health has a tendency to be something a lot of times we don’t want to talk about if it’s not so good. And so just letting people know that it’s okay to. This is kind of. Lots of people have mental health issues. And to be able to connect the dots, you know, like, well, okay, if I need a resource, this is where I can go,” said Glenn Simpson, ECU Health System service line administrator for behavioral health.
ECU Health added that if you or a loved one struggles with mental health issues, you can always call or text the number 988 to be connected with professionals.
The Brody School of Medicine at East Carolina University held its 10th annual Medical Education Day April 25, celebrating scholarship and innovation in medical education.
The event included podium and poster presentations and the popular “Shark Tank” program, during which student presenters have five minutes to pitch their in-progress research to an expert panel and receive feedback on how best to move their projects forward.
Medical Education Day is traditionally a gathering of leaders, educators, students and other scholars that aims to provide a forum for sharing educational innovations in curriculum and teaching, enhances understanding of new approaches in medical education and strengthening the network of Brody community members interested in promoting educational excellence.
“Today marks another significant milestone in our ongoing commitment to advancing medical education and enhancing the quality of health care delivery in eastern North Carolina and beyond,” said Dr. Lisa Domico, teaching assistant professor in Brody toxicology, during opening remarks. “Today we will not only recognize the achievements of our educators, researchers and learners but also remember our dedication to the Brody mission. Our mission drives innovation, excellence and continuous improvement in medical education.”
The keynote speaker was Dr. Andrew Southerland, the Harrison Distinguished Teaching Professor of Neurology and executive vice chair of the Department of Neurology at the University of Virginia Health/UVA Stroke Center. Southerland is a 2006 Brody graduate and was a Brody Scholar. He is the past recipient of an early career award from the American Heart Association/American Stroke Association (AHA/ASA) National Clinical Research Program and has served as principal investigator for numerous clinical studies in the field of stroke and cerebrovascular disease.
Southerland’s address was titled, “Teaching Clinical Diagnostic Reasoning in the Age of AI – Domo Arigato, Mr. Roboto.”
Southerland discussed how artificial intelligence (AI) — which he also called “augmented intelligence” — can improve health care while the importance of a doctor-patient relationship remains at the forefront. He detailed some commercial AI products that contribute to medical care and how they can improve patient and provider experiences.
“I became interested in how we as educators need to consider artificial intelligence when it comes to medical education for the next generation,” Southerland said.
Southerland noted specific examples of products and programs in AI can help physicians better care for their patients. Providers can use AI and build upon its benefits using critical thinking and existing expertise.
“This is what we as humans can do well and how we can think about AI as a way to oversee what it’s doing,” he said.
Students earned accolades for their work during the event. Second-year medical students Jacob Richardson and Alissa Davis won the Shark with the Biggest Bite award for their presentation “Utilization of Artificial Intelligence Image Generation Tools to Augment Mnemonics for Medical Students: Proof of Concept.”
Alexandra Doherty, fourth-year medical student, won the Outstanding Podium Presentation award for her presentation, “A Delphi Consensus Study for the Development of a Specialty-Focused Ultrasound Curriculum for Fourth-Year Medical Students.”
The first-place poster award went to K. Ryan Dickerson, fourth-year medical student and Medical Education and Teaching Scholar, for his project “Near-Peer Created Full Length Practice Laboratory Practicals in Gross Anatomy and Embryology: An Effective Method of Learning in the Anatomical Sciences.”
The second-place poster award went Arden Vessie, fourth-year medical student for her project “Peer-Led Medical Spanish Education: Effects on Interprofessional Student Functional Language Self-Efficacy.”
The third-place poster award went to Michael Kovasala, first-year medical student and Taylor A. Creech, first-year medical student, for their project “Interprofessional Near-Peer-Created Resources in Gross Anatomy: Medical Student Support and Perceived Impact on Emotional Well-Being.”
Dr. Michael Granet has provided more than patient care and dental instruction as an adjunct assistant professor at the East Carolina University School of Dental Medicine’s community service learning center (CSLC) in Brunswick County.
Through gifts totaling more than $100,000, Granet has invested in and helped the school obtain state-of-the-art equipment for the CSLC. Granet, the staff and dental students at the CSLC now have access to a cone beam computed tomography (CBCT)/panoramic X-ray unit, which provides 3D imaging; a TRIOS intraoral scanner and CoDiagnostix software; and a 3D printer. The cutting-edge equipment allows the care team to provide scans for dental imaging instead of having to take impressions.
“Technology is at the forefront of dental education now more than ever before, and Dr. Granet’s gift of this state-of-the-art equipment provides our students and residents with vital exposure to digital dentistry,” said Dr. Greg Chadwick, dean of the dental school. “This gift, coming from a part-time faculty member, leverages our ability to expand the scope of care for the communities we serve.”
Dr. Dianne Caprio, clinical assistant professor at ECU and director of dentistry at the Brunswick CSLC, said dentists can create a virtual model of patient’s teeth or print the model if needed. “Dentistry has gone digital, and we are just scratching the surface of all the possibilities,” Caprio said. “Having this equipment offers the students and residents an introduction to the digital dental world.”
Caprio said the new equipment allows staff the ability to design crowns, dentures and other prosthetics on the software and print them in the office. “We can plan for accurate placement of implants using the CBCT, TRIOS and the CoDiagnostix software by designing surgical guides and printing them in house,” she said.
Granet learned about the CSLC after moving to Wilmington from Maryland. He works at the center each Tuesday caring for patients’ periodontic and implant needs and serving as an instructor for the dental residents working there. “I made donations to the clinic so this equipment could be here and we could all use it and patients could benefit from it,” Granet said. “All I did was give the money. What I get back is much greater than the money I give. I am in a happy place when I get here (Brunswick CSLC) on Tuesday.”
Staff at the CSLC honored Granet for his support with a plaque at the center. Caprio said the upgrade in technology is important to the CSLC, but Granet’s “greatest gift is his time and dedication to teaching the residents and students.”