Blue and silver Pinwheels for Prevention adorned yards, clinics, daycares and other businesses in Greenville, eastern North Carolina and across the country throughout National Child Abuse Prevention Month in April. The pinwheels, meant to represent childlike whimsy and lightheartedness, are a signature display during the month-long campaign to raise awareness around a difficult and important topic.
For team members and supporters at ECU Health and the Brody School of Medicine at East Carolina University’s Tender Evaluation, Diagnosis and Intervention for a Better Abuse Response (TEDI BEAR) and Mt. Olive Children’s Advocacy Centers (CACs), the tireless effort to prevent child abuse in eastern North Carolina is a year-round endeavor.
On Wednesday, April 16, ECU Health’s EastCare celebrated a remarkable milestone: 40 years of dedicated service to the communities of eastern North Carolina. Founded in 1985, the program has grown from a single helicopter operation to a comprehensive medical transport service, offering both ground and air transportation.
EastCare transports patients directly from the scene of an emergency or transfers them from regional hospitals to ECU Health Medical Center, ensuring that critically ill and injured patients receive timely and advanced medical care.
Today, the program operates seven aircraft, with five in use and two back-ups. With eight bases within the region — both ground and air — and 28 ambulances, coverage has expanded to include all of eastern North Carolina as well as parts of South Carolina and Virginia.
You can support the vital services EastCare provides by giving here.
The ECU Health Foundation recently recognized four team members at ECU Health Medical Center with 2024 Brody Awards, on behalf of the Brody families of Kinston and Greenville.
The Brody Awards, established in 1988, are given to team members who demonstrate unparalleled care, compassion, professionalism and commitment in all they do. The awards honor a registered nurse, an allied health professional, a clinical support team member and an Intensive Care Unit nurse.
The 2024 honorees are: Pam Hall, triage telephone nurse in Medical Oncology; Melinda Edwards, trauma registry supervisor; Kaitlin Lehrke, staff nurse II on the Surgical Intensive Care Unit; and Stacey Greenway, former director of Cardiovascular Disease Management.
Access East is a 501(c)(3) that strives to improve health access to, and coordination of, quality care in eastern North Carolina. Access East serves as an important part of the ECU Health system of care, offering support for under- and uninsured individuals and helping navigate the health care system through service lines such as Access East Care Management, HealthAssist, ACA Navigators and Health Opportunities Pilot.
Out in the field
One such facet of their service comes through the Farmworker Program, which works not only to help enroll members of the ENC H-2A (temporary visa) farmworker community in low-cost insurance, but also to direct them to available community health care options, and to provide emergency medical training like wound care or cardiopulmonary resuscitation (CPR). In just under two months, the program has reached more than 2,000 farm workers.
Juan Allen, a community coordinator and Affordable Care Act (ACA) navigator for the program, plays a key role in helping the farmworker community receive the services and care it needs. “I’ve been with Access East for seven or eight years,” Juan said. “I was born and raised in El Salvador on a farm, which is what got me interested in doing this work.” The goal of the program, he said, is to help members of the migrant farming community prevent injuries and illness. “Last year we lost four farm workers to heat stroke, and someone else passed away because no one in the field knew CPR,” he explained.
“So, we go out to the farms and do CPR training, heat exhaustion and heat stroke education, Stop the Bleed training, education about tobacco sickness and anything else they need.” Juan said there is also skin cancer education and screenings, dental cleanings, mental health support and vaccines. “During COVID, we were coordinating vaccines, so that with providers’ help, we got 80-100 people vaccinated per day.”
Juan has also trained as an instructor for the Mental Health First Aid (MHFA) trainings, which is an evidence-based, early-intervention course that, virtually or in-person, uses community-specific scenarios, activities and videos to teach people the skills they need to recognize and respond to mental health and substance use challenges. The ECU Health Foundation awarded funding to Safe Communities Coalition, a non-profit that works alongside the Eastern Carolina Injury Prevention Program (ECIPP) to prevent injuries. “Juan has reached a population (farmworkers) that we have struggled to reach, yet we knew desperately needed the education,” said Sue Anne Pilgreen, the executive director for the Safe Communities Coalition, the manager of the ECIPP and the manager of the Pediatric Asthma Program. “This past fiscal year, we have trained a total of 196 people in MFHA, and 92% felt like they could recognize someone who was suicidal after completing the class.”
“Juan is one of the hardest workers I know,” said Shantell Cheek, the director of Access East. “He has a passion to really help those who are underserved, and he is a true link between Access East, ECU Health and the Farmworker Program.” Wherever there is a need, she said, Access East and the Farmworker Program is there.
The program, which initially was established to help H-2A workers get visas and enroll in the ACA, has grown significantly. “We still do the ACA enrollment,” Cheek said. “But Juan provides care coordination, and different entities like the North Carolina Department of Health and Human Services and the North Carolina Growers Association partner with us. We now help these individuals get medications they need, assist them when they go to the hospital and are being discharged, set up with primary care providers and provide the education like CPR and skin cancer. And it’s not just the migrant workers; it’s their families too. Wherever there is a need, anywhere across the state, they call Juan.”
Partnering with the Brody School of Medicine
She emphasized that Juan tirelessly creates partnerships with regional and community organizations. Shantell also highlighted Access East’s, and Juan’s, ongoing collaboration with East Carolina University’s Brody School of Medicine. “During their first or second year of medical school, students can select a project to work on and Juan’s name often comes up when they mention an interest in the communities we serve.”
Deanna Torres, a second-year medical school student at the Brody School of Medicine, worked with Juan this past summer as a part of a project required of the school’s four Distinction tracks. Deanna opted to apply for the Service-learning track, which is what led her to Access East. The other tracks include Health System Transformation and Leadership, Medical Education and Teaching and Research.
Deanna said she has always had a passion for grassroots community service. “I’m undecided on my specialty right now, but I know I want to help underserved, minority populations.” Deanna grew up participating in a variety of community service activities, including a medical mission to Honduras and a Benedictine Volunteer Corps trip to the Rosebud Indian Reservation in Mission, South Dakota. Once she entered medical school, Deanna continued her journey in service by joining the Service-learning track. “It isn’t required to join a track,” Deanna explained. “But when I was applying to medical schools, the Service-learning track was a major factor in deciding to come here.”
Students in the Service-learning track work extensively with medically-underserved, marginalized and rural populations during their medical school career. They attend a lecture series specific to that track, but they are also required to participate in a service-learning internship during the summer after their first year of medical school. “We select an organization to partner with, and then we create a longitudinal service-learning project aligned with that organization,” Deanna said. While the internship only lasts a summer, the students’ work on their projects continues until they graduate.
Making a difference
With Juan as her mentor, Deanna said she gained an insider’s perspective on a migrant farmworker’s daily life. “I saw how migrant farmworkers are processed after entering the country. I saw how farms are laid out, and I got to see their living conditions, which aren’t always great. I’ve lived in North Carolina my whole life, and I didn’t know how many farmworkers we have in this region or what their needs were.” This exposure led Deanna to her project’s focus, which is “Increasing Mental Health Services to Hispanic Migrant Farmworkers in Pitt County.” The migrant workers, she discovered, often struggle with mental health issues, like depression. “They leave their home country and their families, work in the heat and have no car or independence, and that can be challenging. I want to advocate for the lack of awareness and communication about mental health in the Hispanic community,” Deanna said.
Juan has been instrumental in helping Deanna make the connections and partnerships necessary to work on her project. “He’s a popular man,” she laughed. “Any time I mention Access East, everyone knows him.” Deanna said she appreciated Juan being willing to mentor her, despite his busy schedule. “As a medical student, it can feel daunting to reach out because everyone is busy, but he was always available and offered me resources, took me to the farms and provided logistics. He knows all about these things.”
Dr. Jennifer Crotty, a pediatrician and an associate professor in the Department of Pediatrics at the Brody School of Medicine, as well as the director of the Service-learning distinction track, facilitates connections between students in the Service-learning track and community partners. “The track primarily focuses on local impact and grassroots efforts,” Dr. Crotty said. Of how she came to direct this specific track, she cited her background in pediatrics. “I realized that to have healthy children, we need healthy families and communities,” she said. “That’s why we want to do this advocacy work.” Access East has been a significant partner in this work. “Access East addresses the things we know need to be addressed. When students work with them, they see the time and energy and resources it takes to do medicine in these rural communities.” While she has never met Juan personally, she knows her students get a great experience when they work with him. “He always finds a place for our students, and the students always say their experience was amazing.”
This work is valuable, Deanna said, because it puts a face and name to abstract medical concepts students learn in school. “It puts a story to what you’re learning,” she said. “It shows us that a patient isn’t just one disease, but they are dimensional, and it helps us be better physicians who treat in a holistic manner. This community needs us to advocate for them.” Dr. Crotty agreed, saying that having students participate in these service learning partnerships through ECU Health make them better physicians, no matter what specialty they choose. “They take the knowledge they gained through service learning to wherever they’re going. I love that someone in their surgery residency is thinking about whether their patient has enough food at home. We graduate good doctors because our students are exposed to these types of things, and they know how to handle it.” Juan said that ultimately, this work gives migrant farmworkers a voice. “They’re only here for eight months and they don’t know their rights,” he said. “Access East is vital to reach out to farm workers so we can be a go-between them and the health system.”
It’s not just in October, which serves as Breast Cancer Awareness Month, that you can find the ECU Health Cancer Care Outreach team making connections in the community.
Jennifer Lewis, outreach coordinator for cancer care at ECU Health Medical Center, said she spends much of her time reaching out to community partners, talking to groups in Pitt County and beyond, and connecting with ECU Health patients and families. However, she said, the most rewarding part of her job is the monthly free breast clinic she helps run.
The clinic, for women in Pitt County age 40 and older who are low income and do not have health insurance, provides screening mammograms while sharing other resources available for health care in the area with those participating in the screening.
Lewis said she is grateful to help with the program and is proud of the impact it has on Pitt County.
“Patients don’t see a bill because of donations to the Cancer Center and the ECU Health Foundation, and that’s just an amazing thing we get to offer,” Lewis said. “We start with a breast exam by a provider to check for obvious abnormalities. Then they have their 3D mammogram, so they get state of the art imaging just like anyone else would get and they don’t get lesser quality. If they have an area that is of suspicion, we can do a diagnostic mammogram and if the radiologist looks at those images and feels like there’s some more concern about something, next would be an ultrasound of that area of suspicion. The program that we have here pays for all that.”
She shared that while ECU Health Beaufort Hospital and Outer Banks Health currently have their own programs outside of Greenville and Pitt County, other hospitals across ECU Health’s system are working toward establishing the program as well.
Lewis said the partnerships and volunteerism associated with the program make it truly special. She and her team work closely with the Pitt County Health Department to help patients who need further care through the Breast and Cervical Cancer Control Program (BCCCP).
“We can’t do this without our partners, that’s for sure,” Lewis said. “We have such a great working relationship with the Pitt County Health Department and the mammography technicians, Patient Access Services, Language Access, Volunteer Services, radiology and ultrasound, and then our nurse residents who help out all work together so well. After patients are seen during the free clinic day, we have Access East on hand, too, to share information and resources about other services they can get access to. It’s such great teamwork all around that makes these events successful.”
The program sees so many patients throughout the year that they’ve recently added an extra clinic day twice a year, once in February and once in October, to help meet the needs of the community.
While Lewis is frequently in the community talking to groups and spreading awareness, October is especially important. She said she’ll spend much of the month meeting with community groups and in churches discussing risk factors, signs and symptoms and why screenings are important.
“This month is an intentional time set aside to speak about risk factors, family history, and signs and symptoms, because that’s the one time of the year that you can sit back and think, ‘OK, am I having any of these symptoms?’ Or ‘What is my family history? Because last year I didn’t have any, but this year my mother or sister has been diagnosed with it.’ It really creates that intention for people to have that moment sometime during the month,” Lewis said. “Whether it’s an ad on Facebook or hearing someone like me speak, it’s important to have that moment of reflection, remind yourself to get a mammogram and just put that in the forefront of women’s minds.”
She said if there’s one thing she could remind the community, it’s that anyone can be diagnosed with breast cancer. She noted that there are many myths, including that because someone is without family history, is otherwise healthy or is a male, that they cannot develop breast cancer. This is why she said it’s critical for everyone to be aware of signs and symptoms and receive screenings as recommended.
Resources
Breast Screening Events
ECU Health Cancer Care
More Breast Cancer Information
Healthy snacks, well-being resources, a mindful walking trail and more were all on display at ECU Health Medical Center’s new Resident Well-Being Zone as part of a recent pop-up event hosted by ECU Health’s Well-Being team.
Resident physicians from across the Medical Center were invited to the pop-up event as a way of showcasing the new space, intentionally designed to support their well-being as they continue in their journey in medical education.
The pop-up event, according to Dr. Christina Bowen, ECU Health’s chief well-being officer, is an important way of ensuring residents are aware of the resources available to them at ECU Health.
“We are thrilled to have a resident well-being zone and to be able to offer something unique and purposeful to our resident physicians, who play such an important role here at ECU Health Medical Center,” said Dr. Christina Bowen, Chief Well-being officer at ECU Health. “The pop-up events are a fun way to get our resident physicians engaged in well-being and mindfulness which we know will benefit them during their time here at ECU Health. Our team is excited to be able to host well-being events throughout the year.”
Located on the sixth floor of the Eddie and Jo Allison Smith Cancer Center at ECU Health Medical Center, the Resident Well-Being Zone officially opened in August after years of thoughtful design and funding provided by the ECU Health Foundation. The space is filled with all the essentials a resident may need: exercise equipment, charting space, healthy snacks, coffee, even a ping-pong table and more.
Dr. Cole Carter, a fourth-year physical medicine and rehabilitation resident, said the pop-up event and the space itself have proven to be a welcome asset in the resident experience at ECU Health.
“I think it’s great,” Dr. Carter said, noting that his favorite part of the space is the ping-pong table. “It’s a great place to check out when you need a break from the busy schedule. You can get a great view of Greenville and just take time to relax. I try to come up here once a month or so. This is a great asset for our residents and for those who may be looking for a residency program.”
Dr. Mary Catherine Turner, interim associate dean of Graduate Medical Education, understands first-hand the value of a Resident Well-Being Zone. She said she was fortunate to have one during her time as a resident physician, and it helped her take a break, refresh her mind and get re-engaged in the mission-driven work of providing high-quality health care. Now, she is excited that current and future resident physicians get to experience a similar benefit as they care for patients and continue to learn at one of the busiest academic medical centers in the nation.
“A space like this is important for residents,” Dr. Turner said. “Residents need a place where they can go and disconnect from their work for a little bit and reconnect with themselves. And importantly this is a place where residents can congregate together. I think there’s a lot that can be said for building a community, and this allows them the space to do that.”
On Aug. 28, East Carolina University College of Nursing and ECU Health gathered to celebrate their academic-practice partnership. Topics of discussion included entry-level and graduate-level education and practice, nursing research, and their vision for the future.
Chief Nursing Executive of ECU Health, Dr. Trish Baise, appreciates all the work that has been done by the collective nursing leadership team over the last few months. “We have built a strong foundation and are already realizing outcomes. This is just the beginning. Both our institutions are committed to finding innovative partnership opportunities that support the needs of our region and a better future for eastern North Carolina.” Baise said.
Dr. Bimbola F. Akintade, dean and professor at ECU College of Nursing, reflected on the past and mentioned that both institutions have come a long way.
“One of our advantages is not just the proximity but the overarching institutional dynamic we share can only serve as resources. Our vision is that both institutions are so intertwined that students who are graduating from ECU will also see an opportunity to work at ECU Health,” Akintade said.
Graduate-level education programs such as the Adult-Gerontology Clinical Nurse Specialist and the Neonatal Clinical Nurse Specialist concentrations are advancing nursing practice to provide better care for eastern North Carolina. The Clinical Nurse Specialist (CNS) program is unique and the only one in North Carolina. In addition to graduate-level programs, ECU and ECU Health have collaborated to sponsor a nurse extern program. This immersive program, allows students to gain practical experience in various care settings across the health system before their final semesters of nursing school.
During the celebration, a recent graduate of the nurse extern program expressed her gratitude. “I have never been more sure that I am where I’m supposed to be as a nurse and here at ECU Health,” she said. Kiley Fisher will be joining ECU Health Medical Center in February 2025.
Both institutions are hopeful for the future and what is to come.
Dr. John Catanzaro, professor and chief of the Division of Cardiology at the Brody School of Medicine at East Carolina University and director of the East Carolina Heart Institute at ECU Health Medical Center, was recently honored with the prestigious Dr. John “Jack” Rose Distinguished Professorship, recognizing his significant contributions to improving health care delivery, excellence in clinical medicine, administration and academic advancement, including formation of the first Clinical Cardiac Electrophysiology Fellowship at ECU Health.
The Rose Professorship, established by ECU Health and East Carolina University through the ECU Health Foundation and state funds, honors Dr. Rose, a renowned cardiologist and professor. This endowed title supports the director of the East Carolina Heart Institute recognizes Dr. Rose’s exceptional contributions to cardiology and medical humanitarian work. Dr. Rose, who joined ECU Health in 1982 and the Brody School of Medicine in 1990, is celebrated for his dedication to patient care, teaching, and community service. Recipients of this professorship are expected to embody his ideals and passion for teaching, inspiring future generations of medical professionals.
“It’s an honor to be named to the Rose Professorship,” said Dr. Catanzaro. “This title not only recognizes Dr. Jack Rose’s work and legacy, which is focused on humanitarianism and the humanistic qualities of medicine, but it also allows me to highlight and continue his remarkable contributions. As program director, I perform hands-on teaching with trainees during cardiac procedures as well as teach didactic sessions. My primary role is to train the next generation of electrophysiologists to increase access to the patients of eastern North Carolina while maintaining a high standard of excellence in administration and leadership. This professorship is an opportunity to advance Dr. Rose’s legacy of teaching, administration and leadership, ensuring that his impact endures in these areas.”
Dr. Catanzaro completed his Doctor of Medicine with distinction in research at SUNY Downstate Medical Center, followed by an internal medicine residency and cardiovascular disease fellowship at North Shore University Hospital and a clinical cardiac electrophysiology fellowship at The Johns Hopkins Hospital. He also holds an MBA from the University of Florida. He is a Fellow of the American College of Cardiology, Heart Rhythm Society European Heart Rhythm Society and European Society of Cardiology. Dr. Catanzaro is actively involved with the Heart Rhythm Society’s Atrial Fibrillation Stroke Prevention Task Force and serves as vice chair of their Quality Improvement Committee. Nationally recognized for his work, Dr. Catanzaro has delivered invited presentations and chaired panels in the U.S., France, Italy, Germany, England, Romania and more. He also performed recorded procedures for the Heart Rhythm Society Scientific Sessions.
Dr. Catanzaro wanted to transition to an administrative role to broaden his impact beyond individual patients to the entire region and the cardiology division.
“We thought he was the best person for the future of cardiology,” said Dr. Mark Iannettoni, W. Randolph Chitwood, Jr, MD, Distinguished Chair in Cardiovascular Sciences, Brody School of Medicine at ECU and chief, Cardiovascular Service Line at the East Carolina Heart Institute at ECU Health Medical Center. “Dr. Catanzaro possesses a highly entrepreneurial spirit, bringing significant innovation to ECU Health. He has developed new techniques and devices in electrophysiology, advancing our capabilities in device management and patient care.”
The Rose Professorship comes with an endowment, managed by the university, to support ongoing and future initiatives in medical education and innovation. The endowment provides approximately $64,000 annually to advance the cardiology division’s educational and innovative efforts, supporting activities such as purchasing educational equipment, facilitating attendance at conferences, and other educational pursuits.
“The professorship facilitates innovation within the field by providing the necessary funding for new initiatives, such as introducing new devices,” said Dr. Catanzaro. “The goal is to use a certain amount of the endowment each year to support these innovations and to produce more trained physicians for the region. This helps establish our institution as a center of excellence and makes our advancements known.”
Dr. Catanzaro utilized part of the endowment to establish a two-year Electrophysiology Fellowship, admitting one fellow per year, starting this year. Electrophysiologists treat heart rhythm disorders and heart failure with electric devices inserted into the heart. As part of the fellowship, doctors will learn about pacemakers, defibrillators, implantation, ablations, leadless pacemakers, and left atrial appendage closure devices.
“This was one of the fastest fellowships from concept to establishment that we’ve ever done, which just goes to show you how much drive Dr. Catanzaro has,” said Dr. Herb Garrison, former associate dean for ECU’s Brody School of Medicine Graduate Medical Education. “It typically takes two to three years to establish a new residency or fellowship, and we did this in less than a year. That was a record time. And part of that had to do with Dr. Catanzaro and Alyson Riddick, who did an excellent job putting the application together.”
Dr. Jan Lopes is the first fellow in the Electrophysiology Fellowship at ECU Health. He learned about the new program through his cardiology fellowship leader in El Paso, Texas, and decided to join the fellowship because of Dr. Catanzaro’s strong vision for the program.
“Dr. Catanzaro’s enthusiasm for the program and education, along with the opportunity to shape the program for future fellows, attracted me to the fellowship,” said Dr. Lopes. “Despite being a new program, it feels well-established and highly developed. I feel incredibly supported in my role and am receiving top-tier training that rivals what is offered at major medical centers nationwide. We are utilizing cutting-edge technology and performing the latest procedures here at the medical center.”
Training doctors like Dr. Lopes with the latest technology and procedures is important for the future of health care. The need for well-trained electrophysiologists is increasing across the nation and here in eastern North Carolina, according to Dr. Garrison.
“The incidence of arrhythmias, along with the need for pacemakers and defibrillators, is rising as the population ages, making it a critical area of focus,” said Dr. Garrison. “Establishing residencies and fellowships serves two main purposes: recruiting top-tier faculty and creating a pipeline of skilled electrophysiologists. Faculty are attracted to institutions with trainees, and enhancing our program with excellent faculty was a strategic move by Dr. Catanzaro. This initiative ensures we have the necessary capability and qualified physicians to meet the growing demand for electrophysiology services.”
With the increasing demand for physicians and electrophysiologists trained to treat rural patients, Dr. Catanzaro’s efforts at ECU Health is paying off in the form of improved recruitment efforts.
“Dr. Catanzaro has successfully attracted numerous cardiologists,” said Dr. Iannettoni. “He has excelled at developing divisions within the cardiology department and navigating the integration of academia and medicine. His efforts have resulted in many of our graduates choosing to stay with us, which is a significant benefit of our program. We’re proud to retain our own trainees, ensuring continuity and excellence in our team.”
Chris Smith, the vice president of finance and operations for the ECU Health Foundation, was working out at the ECU Health Wellness Center when the director pulled him aside and told him about the Rock Steady Boxing program – a non-contact, boxing-inspired fitness routine specifically created for patients with Parkinson’s disease and similar movement disorders.
“They were looking for help with starting up the program – equipment, training for a few coaches, that sort of thing,” Smith said. “I told him we’d take a look at how the Foundation could help, and as it turned out, we were able to provide them the funds they needed to get the program started.”
Parkinson’s disease is a neurological disorder that causes unintended or uncontrollable movements, such as shaking, stiffness and difficulty with balance and coordination. Symptoms worsen over time, causing difficulty with walking, talking or other daily activities. While there is no cure, physical activity can improve many symptoms of Parkinson’s disease, slow the progression of the disease process and improve patients’ quality of life.
A Rock Steady Boxing Program participant works with an ECU Health team member during a training session.
First created in Indianapolis in 2006, Rock Steady Boxing is now an international nonprofit program with more than 840 certified affiliates. Now, ECU Health’s Wellness Center counts itself among those numbers because of the Foundation’s support.
Smith said it was gratifying to know that money given by donors was used in such a meaningful way.
“This demonstrates the impact of what our donors do for their friends and families in the region. It showed the tangible impact philanthropy has on the lives of people in eastern North Carolina.” Smith also had a personal connection to the program; his father had Parkinson’s. “He passed away right before the pandemic. He was doing rehab, but he could never get back on his feet.”
With those donor-provided funds, which covered the cost of coach training in Indianapolis and the necessary equipment, the ECU Health Wellness Center was able to establish a Rock Steady Boxing program in 2023. Two of the coaches trained for the program were Kiara Robins, the lead exercise specialist, and Cas Costa, an exercise physiologist II. More than 36,000 people live with Parkinson’s disease in North and South Carolina, and Costa highlighted the value of having this program in the area.
“I didn’t realize at first the impact it would have, and I didn’t know how few locations offered the class.” That’s true; the ECU Health Wellness Center is currently only one of three locations to offer the program in eastern North Carolina. As a result, Robins said that their class has grown quickly: “We started with just three or four members but now we’re up to ten or twelve. We have people come from Rocky Mount, Kinston, Grimesland, Snow Hill and Ayden looking to do the program. We’re steadily growing, and we’re seeing great results.”
Those results are measured through balance and gait tests, such as the Berg Balance test and the Get up and Go test. “Our first four participants have gone from high fall risks to medium or low risks,” Robins said. “Some couldn’t even complete components of the tests, but they now can.”
Justin Mendoza, one of the participants in the class and its youngest member, attested to the program’s positive effects. “They [the coaches] really put their heart into thinking of exercises. You have someone who has studied this and knows what you’re going through. I’ve improved in my strength and walking, and I don’t fall as often,” he said.
While some clients, like Mendoza, heard about the Greenville class when theirs shut down, others received referrals from their physical therapists or physicians. Dr. Temitope Lawal, an ECU Health movement disorder neurologist, is one of those doctors to refer patients to the program.
“Exercise slows the progression of Parkinson’s,” he said. “It’s an extrapolation of the saying, ‘if you don’t use it, you lose it.’ This program makes you accountable and asks you to move your muscles as much as you can.” Dr. Lawal also noted the social value of the program. “It’s an avenue for interaction with others who have Parkinson’s, so it’s like an informal support group.” Costa agreed: “The biggest benefit is the sense of community. It’s hard to go to a regular gym and know what to do. But here, everyone has Parkinson’s so there’s a level of comfort with the activities.”
That accessibility to specialized exercise programs is just one of the things that sets apart the ECU Health Wellness Center.
“The Wellness Center is more than a gym,” Robins said. “You have trained staff here, all with a degree in exercise and certified in one or more areas to better serve the population.” Costa also emphasized the value of specialty-trained staff. “We’re a wellness center, which is different from a gym. In a gym you can’t see a dietician or a lifestyle coach or go next door for a physical therapy appointment. We have a full-circle of wellness with staff trained to help patients with Parkinson’s, arthritis, orthopedic needs, cancer and other diagnoses.”
Both coaches acknowledged that collaboration is required to make Rock Steady Boxing and other programs successful.
“I’m working towards a Ph.D. in kinesiology, and in school we’re learning about the relationship between physicians and exercise physiologists,” said Costa. “Rock Steady Boxing is an example of that collaboration. ECU Health supporting this program helps us build relationships with the doctors and specialists in the network.”
This partnership provides access to valuable resources and complements the medications patients with Parkinson’s must take to combat the symptoms.
Membership is not required to participate in Rock Steady Boxing. “90 percent of our participants are non-members,” Robins said. Participants pay for eight sessions per month, but there’s also a drop-in rate for those who have less predictable schedules. Those who are unsure if they want to join can observe a class for free, and they can participate in the class on a month-to-month basis with no obligation.
Robins said the program has plans to continue its growth so it can better serve the region, and both she and Costa shared their appreciation to the Foundation for supporting the program.
“We’re grateful to have this program here in Greenville,” Robins said. “We’re still in the beginning stages, but we want to expand as much as we can and get more members. We want to encourage everyone with Parkinson’s to participate and to let them know we’re here to help as much as we can.” Mendoza championed the program and the coaches for their hard work: “I love the class. We have fun, and the coaches know what they’re doing. You don’t feel intimidated or self-conscious, and it gives you a sense of pride.”
Just being a kid – that’s the goal Camp Hope and Camp Rainbow staff hope to accomplish every summer. Each year ECU Health and the Department of Pediatrics Hematology/Oncology at the Brody School of Medicine make it possible for children with cancer, hemophilia and sickle cell disease to take part in summer camp.
Camp Rainbow is for children with cancer, hemophilia and children who have lost a sibling to one of these diseases, and Camp Hope is for children with sickle cell disease.
“Once the kids get to camp, start participating activities and get to know each other, they leave everything behind and just get to be kids,” said Jacque Sauls, child life specialist at the Pediatric Hematology/Oncology Clinic at ECU Health and the Brody School of Medicine at East Carolina University and director of Camp Hope and Camp Rainbow. “That is a blissful moment for all of the health care staff to be able to watch a child we see in the hospital all the time being a kid and having a great time.”
ECU Health and Brody team members develop camping programs to provide pediatric patients an opportunity to learn more about themselves and their illness, participate in fun activities like swimming, canoeing, archery, crafts, music and drama, all while making life-long friendships with other children with similar conditions and experiences. Over 60 campers from 25 counties in eastern North Carolina came this year.
“These kids are often protected and sheltered a little bit because they can’t do all the things other kids can do because of their illnesses, or they’re afraid of infections or normal camps don’t have the health care they need,” said Sauls. “Here, they can do every camp activity. There are no limits.”
While at camp, children receive 24-hour medical care and close medical monitoring by their ECU Health care teams including physicians, nurses, child life and social workers.
“All of the children take medicine because of their conditions, so when they take it together, they realize, ‘You have to do this just like I do,’ and know they’re not alone,” said Sauls.
The vast majority of camp volunteers and counselors are former campers themselves, having experienced sickle cell, bleeding disorders or cancer. This shared background allows them to form a special connection with the campers, having faced similar challenges, treatments and experiences. These volunteers return to camp to ensure that today’s kids receive the same transformative experience they once did.
“It’s one of the most important things we do at camp because they get to meet children going through the same thing they’re going through or have gone through,” said Sauls. “The kids get to have mentors that have gone what they’ve gone through and are now in college. They get to see that just because you have a chronic illness or have had cancer you can’t do all the things you want to accomplish in life.”
This is true for camp volunteer Daniel Everett, who attended Camp Hope starting in 2017. When he graduated high school in 2021, he decided to volunteer at the camp.
“I have sickle cell myself, and for me as a kid to come to camp was a dream,” Everett said. “It was magical. It was a place I could go that I knew I was going to have fun, and it was a place I felt right at home.”
Now as a counselor, Everett makes the same impact on the new campers.
“It’s really awesome seeing the kids enjoy themselves, especially when they come from a background of pain, they may be going through treatment,” Everett said. “It’s just nice to see them come here to take a breather like, ‘I can be myself,’ because they’re accepted here.”
Everett is beginning college in the fall, and Sauls noted how important it is for the campers to see someone with the same disease as them accomplishing their goals.
One volunteer, however, is not a former patient. Dr. Ashish Khanchandani recently graduated from the Brody School of Medicine at ECU and is beginning his residency in Pediatrics at ECU Health Medical Center. Dr. Khanchandani volunteered during his gap between medical school graduation and residency to make sure the campers have fun and to assist in any medical needs the campers may have.
“The goal of us as volunteers is to make sure the kids can go about their day without any major medical issues,” Dr. Khanchandani said. “It has been fun being like a camp counselor. I’ve done all the activities with my kids like paddle boarding, all while making sure they’re doing it safely.”
Sauls said she was especially grateful for Dr. Khanchandani’s expertise when it comes to his group of campers. His group has Daniel Perez, a camper who survived brain cancer at two years old, losing his vision. Perez was diagnosed with bone cancer in his leg at age nine and underwent chemotherapy. Thanks to the help from Dr. Khanchandani and another camper named Esra Lupton, Perez has been able to participate in every single activity.
“Daniel and Esra met at this camp for the first time, and they go everywhere together,” said Sauls. “Esra takes him from place to place. It’s a friendship you would never be able to make somewhere else.”
Perez, like the other campers, has loved his time at Camp Rainbow. He said coming to camp helps him de-stress and forget about the medical stress going on his day-to-day life.
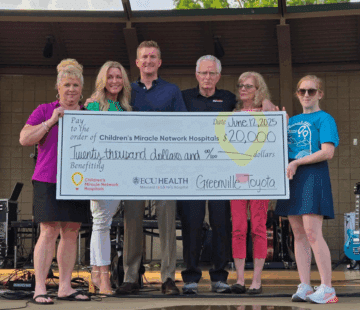
Camp Rainbow and Camp Hope are offered free of charge to children with chronic illnesses and were made possible this year by generous support and donations from the ECU Health Medical & Health Sciences Foundation, Inc., Children’s Miracle Network Hospitals/ECU Health Foundation, the Pamlico Neuse Women’s Coalition, the James and Mamie Richardson Perkins Trust, the Mildred Sheffield Wells Charitable Trust, Riley’s Army, Jaylen’s Nation, Ms. Tammy Thompson, Beau’s Buddies, China Kitchen of Robersonville and other individuals and civic organizations. To learn more, please visit: https://pediatrics.ecu.edu/camp-rainbow/